Neuropathic Pain
Neuropathic Pain
Pain is an unpleasant sensory and emotional experience that can have a significant impact on a person's quality of life, general health, psychological health, and social and economic wellbeing (NICE, 2017).
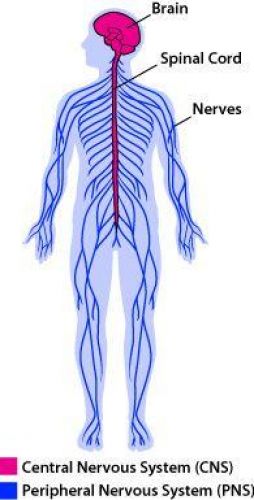
Neuropathic pain is a type of persistent (or chronic) pain caused by problems with the nervous system. This is the part of your body that helps you feel touch, pressure, pain, temperature, position, movement, and vibration. This can be in your muscles, joints, skin, and the layers of tissue just beneath your skin (fascia).
What Causes Neuropathic Pain?
Neuropathic pain can be due to problems with your central nervous system (your brain and spinal cord) or your peripheral nervous system (wider nervous system outside of the brain and spinal cord). Sensors send signals from the skin and body tissues to the spinal cord and brain, where they are registered as pain.
Sometimes, pain can occur on its own (without an obvious "trigger"). Other times, it may be caused by cold, heat, gentle pressure on the skin, or other stimuli that are not usually painful. People with neuropathic pain often have difficulty sleeping. This can lead to fatigue, and for some people, depression.
How Is Neuropathic Pain Treated?
Neuropathic pain can be difficult to manage, because it has a wide range of causes. These can include previous illnesses, existing conditions, surgery, or acquired injury. The pain can come in short bursts, or it can be there all the time. It can feel like shooting, stabbing, like an electric shock, burning, tingling, tightness, numbness, prickling, itching, or a sensation of pins and needles.
We are not sure how many people suffer from this sort of pain. Estimates suggest around 7 people in every 100 may experience these symptoms.
If you develop this sort of pain, it is important to ensure any underlying conditions are being managed as well as they can be. For example, if you have diabetes, your GP should ensure that it is under control. Once this is done, you may be prescribed medication to help with the pain, or you may be referred to PPSS, where our specialist physiotherapy and psychological programme and our pain medication specialist can help you to manage your pain.
When agreeing a treatment plan with you, your GP may discuss with you:
- How bad the pain is
- Its impact on your lifestyle, daily activities (including sleep disturbance) and participation
- The underlying cause of the pain, and whether this condition has got worse over time
- Why a particular painkiller is being offered
- The benefits and possible side-effects of painkillers. This should take account of any physical or mental health difficulties you may have, and any other drugs you are already taking
- The importance of understanding how you respond to the drugs and how the dosage may need to be changed over time to ensure you take the correct amount. This will be specific to your own situation
- How you can learn skills to cope with the pain, and any possible side-effects of the treatment
- Other non-drug based options you may have. This may include a referral to the PPSS.
Painkillers for Neuropathic Pain
Sometimes painkillers are used to help manage this sort of pain. Because of the range of causes and types of pain, it can be difficult to find the right drug to help with your pain. Sometimes drugs are used alone, and sometimes they work better when taken alongside other drugs. Further research is needed into how effective some of these medications are; some have been shown to cause harm in treating some conditions. As your body gets used to certain medications, you may need to take a higher dose to get the same level of pain relief. This is called tolerance, and can lead to you taking more painkillers than is good for you.
So that harmful or ineffective drugs are not used, your GP will try a limited number of painkillers if they feel you need pain relief in the short term to help you manage your symptoms.
For most neuropathic pain, there will most likely be a choice of Amitriptyline, Duloxetine, Gabapentin or Pregabalin as initial treatment. Carbamazepine may be offered as initial treatment for trigeminal neuralgia. If you cannot tolerate taking these medications, Capsaicin cream may be offered instead. These are the only drugs that current clinical research has shown to work, and are recommended for the NHS to use. If you are taking any other drugs, it may be useful to discuss this with your GP, who may refer you to PPSS for a detailed review of your pain medication.
Other Ways of Managing Neuropathic Pain
If these drugs do not help, or you are taking them for a long time, you should be referred to a pain or condition specialist to review your medication and treatment plan. You may be referred to the PPSS, where we can use the pain medication specialist within our team and our specialist physiotherapy and psychological support programme to help you manage your pain.
Whatever form of treatment is right for you, your GP should carry out regular reviews with you to check that the treatment is working. This will include a discussion about:
- Whether the pain is being controlled
- The impact on your lifestyle and daily activities (including sleep disturbance)
- Your physical and mental wellbeing
- Any side-effects you may be suffering
- Whether treatment needs to continue in the same way.
NICE Guidance Neuropathic Pain